An endemic problem in the healthcare industry is that there are too few staff 1 to give all patients the time that they need to receive the best care
Precision medicine is set to revolutionize healthcare,2 and state-of-the-art technologies are essential to achieve this. These technologies will be used to detect patterns in large quantities of genetic, biological, clinical (research), and environmental data, to extract insights related to personalized patient care. Furthermore, an endemic problem in the healthcare industry is that there are too few staff1 to give all patients the time that they need to receive the best care. State-of-the-art technologies have the potential to streamline processes so that healthcare professionals (HCPs) have more time to dedicate to their patients.
When discussing state-of-the-art technologies, we inevitably come across terms like artificial intelligence (AI), machine learning (ML), deep learning (DL), and neural networks (NN). And although we might have a vague understanding of what each of these terms means, it is difficult to distinguish between them and to know how to speak about them when discussing their potential impact on healthcare with colleagues and collaborators. This guide will clarify these terms.
Table of Contents
Artificial intelligence, machine learning, deep learning, or neural networks?
– Artificial intelligence
– Machine learning
– Deep learning
– Neural networks
How are artificial intelligence and machine learning used in healthcare?
– Predictive medicine and imaging
– Patient support
– Health services management
– Physical assistance
– Drug development
How will AI and machine learning impact the future of healthcare?
Conclusion
Artificial intelligence, machine learning, deep learning, or neural networks?
In a nutshell, artificial intelligence (AI) is when computer systems simulate human intelligence by performing tasks that typically require human cognitive abilities.
Machine learning (ML) is one of the key techniques used in AI, where algorithms and statistical models are designed by humans to enable computer systems to learn and improve from experience without being explicitly programmed.
Deep learning (DL) is a subset of ML where algorithms use artificial neural networks to process and analyze large amounts of data, extracting relevant features and patterns.
Neural networks (NN) are a fundamental component of DL algorithms, which are designed to simulate the behavior of the human brain with a network of interconnected nodes (or neurons) that process and transmit information.
For more detailed explanations, click the terms below to reveal.
Artifical intelligence
Although the term AI was coined in 1956 by John McCarthy, the possibility that machines could simulate human behavior and “think” was raised earlier by Alan Turing in 1950.3 Since then, computational power has grown exponentially, and AI is integrated into our daily lives in many forms. For example, many of us use (the likes of) Siri, Alexa, or Google Assistant without a second thought.
More recently, AI has become part of medical practice, where it can improve patient care by speeding up processes and achieving greater accuracy.3 Radiological images, pathology slides, genetic information, and patients’ electronic medical records can be evaluated using AI to aid with administrative tasks and diagnosis and treatment decisions, enhancing the capabilities of clinicians.
Machine Learning
ML is an AI technique for fitting models to data that involves the development of algorithms and statistical models.4 The machine “learns” by training models with data to identify patterns so that it can make predictions or decisions. Machine learning is a widely used AI technique and forms the basis of many approaches within the field.
In healthcare, the most common application of ML is in precision medicine, where patient data are used to predict which treatment strategies are most likely to succeed.4 In order to make predictions, the algorithms generally require a training dataset for which the outcome variable (e.g., onset of disease) is known – this is called supervised learning.
Deep Learning
The most complex forms of machine learning involve DL, or NN models, which have many layers of features or variables that predict outcomes.4 The more layers a network has, the deeper it is, hence the term “deep learning”. The improved capabilities of today’s graphics processing units and cloud architectures make it possible to process and analyze thousands of hidden layers of features.
In healthcare, pattern recognition through DL involves teaching a computer what certain groups of symptoms or radiological images, for example, look like via repetitive algorithms.5 The algorithms enable the computer to learn and improve from experience by adjusting weights and biases. An example of this is when Google’s artificial brain project trained itself to recognize cats based on 10 million YouTube videos, with recognition efficiency improving the more images it reviewed.
DL algorithms can be used for a wide range of applications, such as image and speech recognition, natural language processing, and autonomous systems. A common application of DL in healthcare is for the identification of clinically relevant features (e.g., tumors) in imaging data, which may not be perceived by the human eye.4 Using DL to analyze radiology images can provide a more accurate diagnosis than the previous generation of automated tools for image analysis, computer-aided detection (CAD).
Neural networks
NNs are a fundamental building block of DL algorithms, which can learn and make decisions by themselves.6 They are an interconnected network of nodes (neurons) that mimic the human brain, with weighted communication channels between them.7 Each neuron receives input from other neurons in the previous layer, applies a mathematical operation to that input, and then passes the output to neurons in the next layer. One neuron can react to multiple stimuli from neighboring neurons and use weights and biases to adjust the strength of connections between them. The whole network can change its state based on different inputs received from the environment. As a result, NNs can generate outputs in response to environmental input stimuli, just like the human brain reacts to the environment around us.
How are artificial intelligence and machine learning used in healthcare?
AI and ML can be used in healthcare to assist HCPs in streamlining processes, reducing costs, and perhaps, most importantly, making faster, data-driven clinical decisions, all with the aim of improving patient outcomes. Advances in big data analytics using AI techniques are unlocking clinically relevant information hidden in increasingly available healthcare data, which is successfully assisting HCPs with clinical decisions.8 There are five key areas in which AI and ML are currently accelerating healthcare – predictive medicine and imaging, patient support, services management, physical assistance, and drug development.
Predictive medicine and imaging – supporting quicker and better-informed decision-making
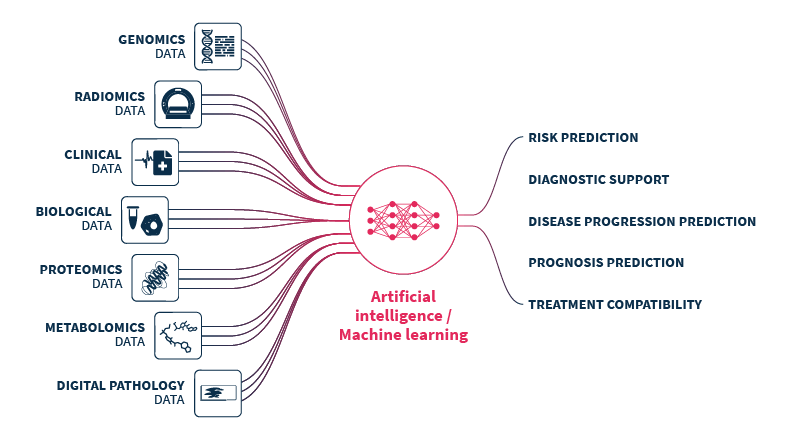
ML has the potential to analyze individual patient data to predict risk, support diagnosis, predict disease progression and prognosis, and to identify the most appropriate treatment regimens.9 In addition, ML has the potential to identify risk factors and drivers for each patient, to help target healthcare interventions for better outcomes.
ML has primarily been used in healthcare to analyze data from imaging, genetic testing, and electrodiagnosis.8 These data are analyzed by AI technologies to cluster patient traits and associate them with a diagnosis, or to predict disease outcomes or response to treatment.
The application of ML to medical imaging has been found to improve accuracy, consistency, and efficiency. In 2017, Arterys developed the first US FDA-approved clinical cloud-based DL application, CardioAI.6 CardioAI analyzes cardiac magnetic resonance images (MRIs) to provide information such as cardiac ejection fraction in a matter of seconds, and has since expanded to cover additional organs and imaging techniques. The time-saving implications from introducing AI support platforms into clinical practice can be quite substantial; radiologists can save ~1 hour per day interpreting chest CTs,10 DL can measure pediatric leg lengths 96x faster than subspecialty-trained pediatric radiologists,11 and AI systems can automate the triaging of adult chest radiographs.12
ML has successfully been used to screen for diabetic retinopathy, identify nonmelanoma and melanoma skin cancers, predict seizures, predict bladder volume, predict cardiovascular risk, and predict progression of Alzheimer’s disease and response to drug therapy.6,7
Patient support – increasing independence and streamlining outpatient care
There are multiple ways in which AI has been used to provide outpatient care. In combination with robotics, AI has been harnessed to restore movement control in patients with quadriplegia for example, and to control prostheses.8 Rehabilitation robots can physically support and guide a patient's limb(s) during physical therapy.9 AI can also be used to assist the independent living of elderly and disabled people with tools such as fall detection systems and wheelchairs controlled by facial expressions.7
AI-powered virtual assistance like chatbots and voice assistants can provide patients with personalized medical advice and support from home, helping patients to manage their own health more effectively with the aim of reducing the workload of HCPs.4,5 Furthermore, wearable systems can support continuous patient monitoring and healthcare delivery.9
Health services management – freeing up more time to spend with patients
AI can support HCPs to work more efficiently, freeing up more time to spend on patient care. AI systems can provide HCPs with real-time medical information updates, coordinate information tools for patients, optimize logistics processes, benchmark data for analyzing services delivered, and much more.9 Process automation, specifically, can be leveraged for tasks such as claims processing, clinical documentation, revenue cycle management, and medical record management.4 Ultimately, the administrative assistance provided by AI creates more time for human interactions.
Physical assistance – increasing precision and efficiency
AI has the potential to transform surgical robotics through devices that can perform semi-automated surgical tasks with increasing efficiency.9 AI technologies can guide surgical tools and make more precise movements than possible within our capacity as humans.5
Drug development – accelerating development and cutting costs
AI techniques streamline the design and development of new drugs by analyzing the vast amount of data available from clinical trials and databases to identify new drug targets and predict drug efficacy and safety.9
How will AI and machine learning impact the future of healthcare?
AI and ML are set to drive the future of healthcare. In particular, ML is a key component in the advancement of precision medicine.4 AI and ML will greatly enhance risk prediction and diagnosis of diseases, and will facilitate personalized treatment strategies based on a broad spectrum of individual patient characteristics. It seems feasible that most radiology and pathology images will soon be examined by a machine and that AI and ML will help HCPs to remotely monitor patients. Speech and text recognition are already used for patient communication and to capture clinical notes, and their usage is likely to increase. AI and ML will also help to accelerate and reduce costs associated with the drug development process.
The successful integration of AI and ML technologies into healthcare requires more than just reliability and accuracy. Several critical factors must be in place to ensure sustainable adoption, including integration with electronic health record systems, standardization, adequate funding, improved regulatory approval processes, staff training, and continuous algorithm optimization with new data.
However, the most crucial factor is transparency. The complexity of AI/ML algorithms and models can make them difficult to interpret or explain, potentially raising concerns about accountability, trust, and privacy. To promote the responsible and sustainable adoption of these technologies, healthcare institutions and regulatory bodies must first establish governance mechanisms and monitoring structures to safeguard the interests of providers and patients alike. This will not only ensure a smooth transition but also foster trust in the use of AI technologies in healthcare.
It seems increasingly clear that AI systems will not replace human HCPs but will instead enhance their capabilities to improve the care of patients. It is important that HCPs are trained and provided with the skills to efficiently work alongside AI. The goal will be to balance a mutually beneficial relationship that leverages on the speed and analytic potential of AI with the uniquely human strengths of empathy, nuance, and seeing the big picture.
Conclusion
Whether AI, ML, DL, or NN, the overall field of artificial intelligence is booming, and the possibilities for improving healthcare are exciting. Although it may seem fantastical, HCPs are already working alongside machines to enhance clinical decision-making, and the future in this field has huge potential for improving patient care.
At SOPHiA GENETICS, we have a strong background in developing ML algorithms that aim to extract actionable insights from genomic data. SOPHiA GENETICS™️ Multimodal Healthcare Analytics (product in development) leverages on propriety ML algorithms, with the potential to maximize the value of multimodal health data. Our technology has so far been utilized in retrospective research studies to assess prognosis and predictive biomarkers in non-small cell lung cancer (NSCLC),13 investigate new meningioma biomarkers to further understand treatment response patterns,14 evaluate pathological complete response status and treatment response in patients with early triple negative breast cancer (TNBC),15 and estimate the risk of disease upstaging, disease-free and overall survival in kidney cancer.16
These studies report data associated with products or concepts in development. They are not available for sale and not intended for use in diagnostic procedures or treatment decisions.
To learn more about SOPHiA DDM™️ Multimodal Healthcare Analytics for the visualization of longitudinal patient data and cohorting, explore here or request a demo here.
References
- Boniol M, et al. BMJ Glob Health. 2022;7(6):e009316.
- Johnson KB, et al. Clin Transl Sci. 2021;14(1):86-93.
- Mintz Y, Brodie R. Minim Invasive Ther Allied Technol MITAT Off J Soc Minim Invasive Ther. 2019;28(2):73-81.
- Davenport T, Kalakota R. Future Healthc J. 2019;6(2):94-98.
- Amisha et al. J Fam Med Prim Care. 2019;8(7):2328-2331.
- Kaul V, et al. Gastrointest Endosc. 2020;92(4):807-812.
- Rong G, et al. Engineering. 2020;6(3):291-301.
- Jiang F, et al. Stroke Vasc Neurol. 2017;2(4).
- Secinaro S, et al. BMC Med Inform Decis Mak. 2021;21(1):125.
- Yacoub B, et al. Am J Roentgenol. 2022;219(5):743-751.
- Zheng Q, et al. Radiology. 2020;296(1):152-158.
- Annarumma M, et al. Radiology. 2019;291(1):196-202.
- Ferrer L, et al. J Clin Oncol. 2022;40(16_suppl):8542-8542.
- Graillon T, et al. Neuro-Oncol. 2021;23(7):1139-1147.
- Groheux D, et al. J Clin Oncol. 2022;40(16_suppl):601-601.
- Boulenger de Hautecloque A, et al. J Clin Oncol. 2022;40(16_suppl):4547-4547.